Keratoconus
What is Keratoconus?
Keratoconus is a common eye condition that affects the cornea – the front window of the eye. The cornea helps to bend and focus light to help us see.
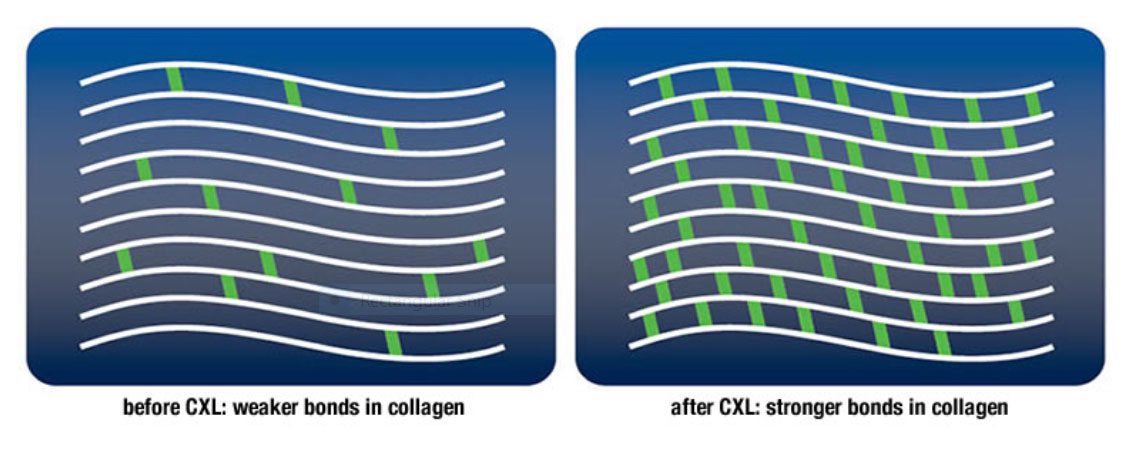
In keratoconus, the cornea begins to thin. As a result, the round shape of the cornea gets distorted, and a cone-like shape develops. The reason for the cornea thinning and coning remains
When the cornea loses its shape, light can’t come to a sharp focus on the retina. This can cause blurry vision, double vision, astigmatism, short sightedness, or light sensitivity. If left untreated, vision will continue to get worse.
In most cases, keratoconus appears between the ages of 16 and 30 years and stabilises by middle age. Due to its early onset, it can impact school, work, social and family life if it’s not treated.
What causes Keratoconus?
The exact cause of keratoconus is not known. But both genetic and environmental factors seem to play a role.
Many people who are affected have no family history of the condition. But it is likely to have a genetic component.
Keratoconus often occurs alongside diseases where people have itchy eyes. For example, hay fever, allergies, and asthma. Lots of vigorous eye rubbing (Knuckle rubbing) can break down the fibres of the cornea. This might increase risk of keratoconus, but the exact link is still unclear.
How is Keratoconus diagnosed?
Patients usually present with blurred vision and sensitivity to light.
A routine eye examination will usually detect astigmatism and reduced vision.
Further investigation using corneal topography and pachymetry will diagnose Keratoconus.
How is Keratoconus treated by an Optometrist?
Initially Keratoconus is treated with spectacles and contact lenses.
Education on avoiding knuckle rubbing of the eyes and using anti histamine eye drops is also crucial to help reduce progression of the condition.
Monitoring of Keratoconus is the key factor to avoiding uncontrolled progression.
If vision cannot be corrected well with spectacles or soft contact lenses, RGP (Rigid Gas Permeable = Hard lenses) can be designed.
If there is progression of Keratoconus, referral to an Ophthalmologist is required.